Gerinnungssystem/en: Unterschied zwischen den Versionen
(Die Seite wurde neu angelegt: „To do this, they are activated by wall collagen fibers that extend into the area of injury. Activation means that they grow larger, that extensions develop fro…“) |
(Die Seite wurde neu angelegt: „https://en.wikipedia.org/wiki/Coagulation“) |
||
| (9 dazwischenliegende Versionen desselben Benutzers werden nicht angezeigt) | |||
| Zeile 13: | Zeile 13: | ||
To do this, they are activated by wall collagen fibers that extend into the area of injury. Activation means that they grow larger, that extensions develop from their wall, and that they attach themselves to the collagen fibers by means of a kind of glue. In doing so, they in turn activate other nearby platelets and thus develop a platelet plug, the so-called primary thrombus. | To do this, they are activated by wall collagen fibers that extend into the area of injury. Activation means that they grow larger, that extensions develop from their wall, and that they attach themselves to the collagen fibers by means of a kind of glue. In doing so, they in turn activate other nearby platelets and thus develop a platelet plug, the so-called primary thrombus. | ||
| − | + | === Primary thrombus === | |
| − | + | However, this plug, the primary thrombus, is not capable of '''permanently''' closing the injured vessel site. This is a good thing, because otherwise small plugs formed too quickly could become a great danger to the circulation. This plug now slowly dissolves again, because it is only there to close smaller wounds immediately. | |
| − | |||
| − | + | == 3rd phase: Secondary hemostasis by clotting factors == | |
| − | + | The complex coagulation system ensures that '''complete''' coagulation occurs only when it is really needed. | |
| − | |||
| − | + | It is activated at the site of injury at the same time that the complex platelet processes are taking place. Its much slower process ends in the formation of [[fibrin/en|fibrin]] threads that weave through the wound plug like a net and are usually also deposited in the immediate vicinity of the plug, including many [[erythrozyt/en|erythrocyte]]s. | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | + | Thus, the occlusive plug now obtains its final strength only by contraction of the platelets ''"matted"'' with their pseudopodia among themselves and with the fibrin threads. | |
| − | |||
| − | |||
| − | + | In this process, which normally takes 5 - 7 minutes (gerinnungszeit/en|clotting time), a '''multitude of plastic factors''' are involved in addition to platelets. Procoagulants and anticoagulants in particular work on this, with the procoagulants naturally having the upper hand in the build-up of the so-called '''secondary thrombus'''. | |
| − | |||
| − | |||
| − | === | + | === Coagulation cascade === |
| − | + | Like primary hemostasis, the actual coagulation process is triggered by vascular and tissue injury and activated by two different pathways: | |
| − | * | + | *exogenous or extravascular pathway ([[extrinsic system]]) - in tissue injury, rapid response. |
| − | * | + | *endogenous or intravascular pathway ([[intrinsic system]]) - in case of injury in the vessel itself, for example [[endothelial]] changes ([[inflammation]]s, [[arteriosclerosis]]), slow response |
| − | + | Thus, on the exogenous pathway, activation occurs very rapidly (within seconds), whereas on the endogenous pathway, the activation process proceeds via a larger number of intermediate steps and requires a longer time (minutes). In the normal coagulation process, both systems are usually involved in an interlocking manner. Through the common final stage of the two activating systems, [[prothrombin]] (Factor II) and with the cooperation of [[vitamin K]] which is formed in the liver, is converted into [[thrombin]]. The resulting thrombin is an [[enzym/en|enzyme]] that cleaves the [[fibrinogen]] (Factor I), which is also synthesized in the liver, and thus initiates the formation of [[fibrin]]. | |
| − | + | The coagulation cascade looks graphically as follows: | |
[[Datei:Gerinnungskaskade_neu.png]] | [[Datei:Gerinnungskaskade_neu.png]] | ||
| − | + | More information: | |
| − | https:// | + | https://en.wikipedia.org/wiki/Coagulation |
Aktuelle Version vom 22. Februar 2022, 12:43 Uhr
The arrest of bleeding, also called blood clotting or hemostasis, is the ability of blood to provide closure to a wound.
blood taken from blood vessels "coagulates" spontaneously within a few minutes in the test tube. During this process, the blood changes from a liquid state to a gelatinous state with the participation of formed elements. The property of blood to clot outside the vascular system is an extremely vital process, the importance of which lies in protecting the body from losing its blood fluid. Blood clotting has several phases
Inhaltsverzeichnis
1st phase: vascular constriction
The blood vessel contracts. This is caused by humorale factors together with neuronal reflexes and locally triggered spasm of the vessel. The vessel closes as far as it can. Now platelets can cluster here.
2nd phase: Primary hemostasis by platelet aggregation
Initially, a wound plug is created solely from the platelets present in the blood:
To do this, they are activated by wall collagen fibers that extend into the area of injury. Activation means that they grow larger, that extensions develop from their wall, and that they attach themselves to the collagen fibers by means of a kind of glue. In doing so, they in turn activate other nearby platelets and thus develop a platelet plug, the so-called primary thrombus.
Primary thrombus
However, this plug, the primary thrombus, is not capable of permanently closing the injured vessel site. This is a good thing, because otherwise small plugs formed too quickly could become a great danger to the circulation. This plug now slowly dissolves again, because it is only there to close smaller wounds immediately.
3rd phase: Secondary hemostasis by clotting factors
The complex coagulation system ensures that complete coagulation occurs only when it is really needed.
It is activated at the site of injury at the same time that the complex platelet processes are taking place. Its much slower process ends in the formation of fibrin threads that weave through the wound plug like a net and are usually also deposited in the immediate vicinity of the plug, including many erythrocytes.
Thus, the occlusive plug now obtains its final strength only by contraction of the platelets "matted" with their pseudopodia among themselves and with the fibrin threads.
In this process, which normally takes 5 - 7 minutes (gerinnungszeit/en|clotting time), a multitude of plastic factors are involved in addition to platelets. Procoagulants and anticoagulants in particular work on this, with the procoagulants naturally having the upper hand in the build-up of the so-called secondary thrombus.
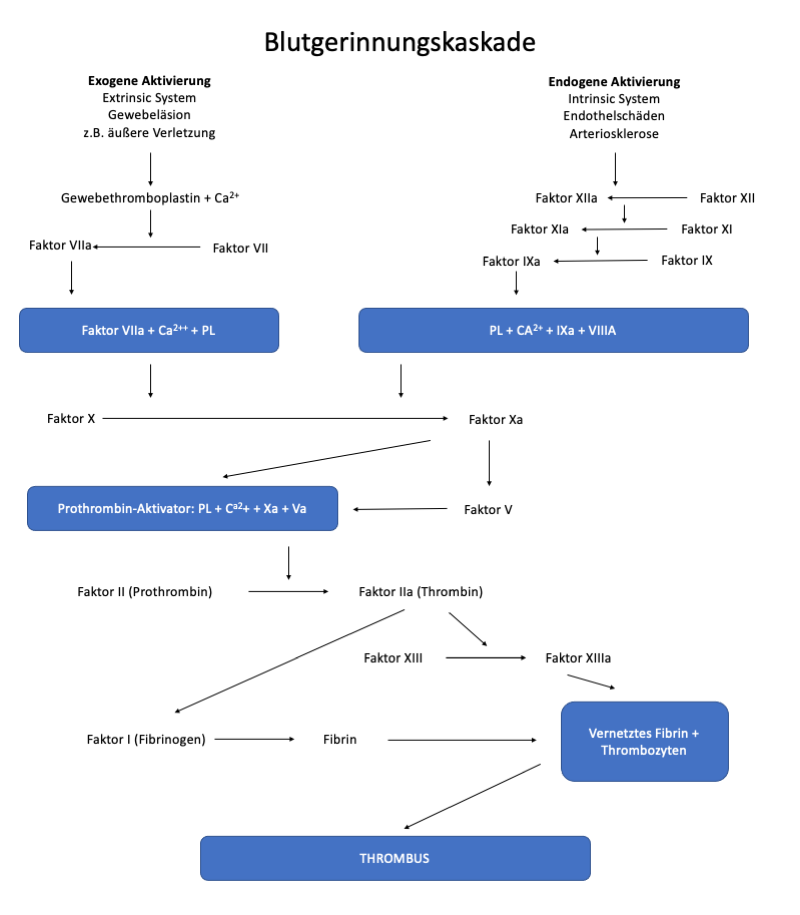
Coagulation cascade
Like primary hemostasis, the actual coagulation process is triggered by vascular and tissue injury and activated by two different pathways:
- exogenous or extravascular pathway (extrinsic system) - in tissue injury, rapid response.
- endogenous or intravascular pathway (intrinsic system) - in case of injury in the vessel itself, for example endothelial changes (inflammations, arteriosclerosis), slow response
Thus, on the exogenous pathway, activation occurs very rapidly (within seconds), whereas on the endogenous pathway, the activation process proceeds via a larger number of intermediate steps and requires a longer time (minutes). In the normal coagulation process, both systems are usually involved in an interlocking manner. Through the common final stage of the two activating systems, prothrombin (Factor II) and with the cooperation of vitamin K which is formed in the liver, is converted into thrombin. The resulting thrombin is an enzyme that cleaves the fibrinogen (Factor I), which is also synthesized in the liver, and thus initiates the formation of fibrin.
The coagulation cascade looks graphically as follows:
More information: